Excessive fluid accumulation within the pericardial space between heart tissues and causes the medical condition of pericardial effusion. The increased fluid inside the pericardial space generates pressure which interferes with heart functionality. When severe pericardial effusion stays untreated it results in the fatal complication known as cardiac tamponade. A stable treatment approach for pericardial effusion demands complete comprehension of its origin, symptoms, diagnostic strategies, and available therapies. A senior heart specialist based in Delhi provides information through the article.
Anatomy of the Pericardium
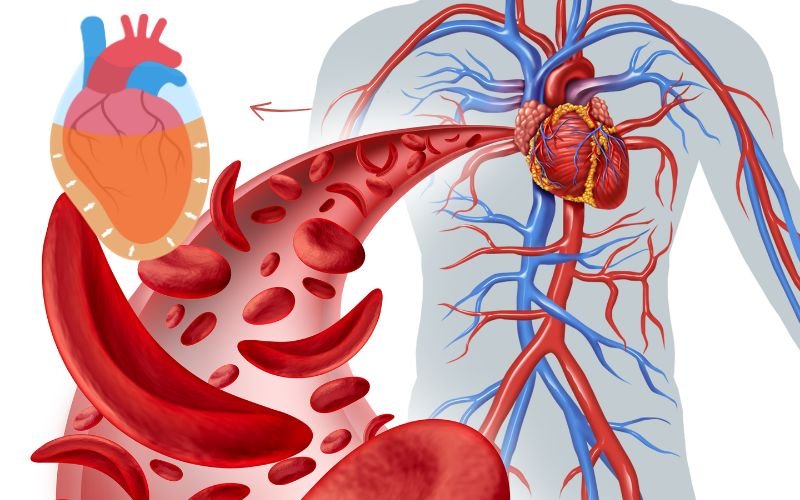
The heart finds protection through two layers of membrane known as the pericardium. It supports heart structure and minimizes friction during each heartbeat. It consists of two layers:
- Fibrous Pericardium: The tough, outer layer that anchors the heart within the chest cavity and protects it from excessive movement
- Serous Pericardium: The inner layer, which is further divided into:
- Parietal Layer: Lines the inner surface of the fibrous pericardium
- Visceral Layer (Epicardium): Adheres directly to the heart muscle and plays a role in producing pericardial fluid
Between these layers lies the pericardial cavity, containing a small amount of lubricating pericardial fluid—typically 15 to 50 milliliters—that facilitates smooth heart movements. However, when excessive fluid accumulates in this space, it leads to pericardial effusion, potentially compromising heart function.
What is Pericardial Effusion?
An abnormal increase of pericardial fluid inside the pericardial sac constitutes pericardial effusion. The volume increase from pericardial effusion can progress from slight to extreme while either emerging slowly or unexpectedly. The type of fluid accumulation within pericardial spaces depends on what causes the condition. The condition sometimes heals naturally but medical treatment becomes necessary for other cases of pericardial effusion.
The severity of pericardial effusion is classified into different types:
- Mild: Small fluid buildup, often asymptomatic
- Moderate: Noticeable symptoms and increased heart strain
- Severe Pericardial Effusion: High risk of complications, including cardiac tamponade
Causes of Pericardial Effusion
Multiple conditions lead to the formation of pericardial effusion. Every treatment requires knowledge of the fundamental source during diagnosis. The main sources resulting in pericardial effusion consist of the following:
- Inflammation of the Pericardium (Pericarditis): Often caused by viral, bacterial, or fungal infections, pericarditis can lead to excessive fluid production
- Autoimmune Disorders: Conditions like lupus, rheumatoid arthritis, and scleroderma can trigger pericardial inflammation and fluid accumulation
- Trauma or Injury: Blunt or penetrating chest injuries from accidents, surgery, or medical procedures such as pacemaker insertion can result in pericardial effusion
- Cancer (Malignant): Metastatic spread from lung, breast, or blood cancers can lead to fluid accumulation around the heart
- Kidney Failure: Uremic pericarditis, a complication of severe kidney disease, can cause fluid buildup
- Hypothyroidism: Insufficient thyroid hormone levels can lead to this disease too.
- Medications: Certain drugs, such as hydralazine and isoniazid, can induce pericardial inflammation
- Radiation Therapy: Cancer treatment involving radiation to the chest can damage the pericardium, leading to fluid accumulation
Symptoms of Pericardial Effusion
The symptoms of pericardial effusion emerge differently depending on the fluid amount and how fast it accumulates along with its root cause. Fluid accumulation affects people differently depending on whether fluid increases slowly or quickly because the symptoms range from nonexistent to potentially fatal
Common symptoms include:
- Chest Pain or Discomfort: Often sharp and may worsen with deep breaths or lying down
- Shortness of Breath (Dyspnea): Occurs due to increased pressure on the lungs and heart
- Fatigue: A general feeling of tiredness or weakness due to decreased cardiac output, It can also be due to cardiomyopathy
- Palpitations: A sensation of rapid, irregular, or forceful heartbeats
- Cough: Resulting from compression of nearby structures, particularly the lungs and trachea
- Low-Grade Fever: Indicative of an underlying infection or inflammatory process
In severe cases, where fluid accumulates rapidly or in large amounts, a life-threatening condition called cardiac tamponade can occur. This condition is characterized by:
- Severe Shortness of Breath
- Low Blood Pressure (Hypotension)
- Distended Neck Veins
- Rapid Heart Rate (Tachycardia)
- Loss of Consciousness
Immediate medical intervention is necessary to relieve the pressure on the heart.
Diagnosis Heart fluid Effusion
Accurate diagnosis is essential for effective management. A heart specialist in Delhi may employ several diagnostic tools:
- Physical Examination: Listening for heart sounds and assessing symptoms such as jugular vein distension
- Echocardiogram (ECHO): A primary imaging test that provides real-time visualization of fluid around the heart
- Effusion X-Ray: May show an enlarged cardiac silhouette due to excessive fluid
- Electrocardiogram (ECG): Helps identify electrical changes, including reduced voltage and electrical alternans
- Computed Tomography (CT) Scan: Provides detailed cross-sectional images of the pericardium and heart
- Magnetic Resonance Imaging (MRI): Offers high-resolution images and helps assess the nature of pericardial effusion

Risk Factors for fluid accumulation in heart
Several pre-existing health conditions and particular lifestyle factors increase the probability of pericardial fluid in heart development in people. The key risk factors include:
- Chronic Infections – Conditions like tuberculosis and HIV increase the risk of pericardial inflammation
- Autoimmune Disorders – Patients with lupus, rheumatoid arthritis, or scleroderma have a greater chance of developing pericardial fluid buildup
- History of Radiation Therapy – Patients who have undergone radiation to the chest area for cancer treatment may develop pericardial scarring, leading to fluid accumulation
- Previous Heart Surgery – Individuals who have undergone procedures like open-heart surgery or valve replacement are at risk of post-surgical pericardial effusion
- Chronic Kidney Disease – Those with renal failure may develop uremic pericarditis, leading to pericardial effusion
Identifying these risk factors can help in early screening and preventive care.
Treatment Options for Pericardial Effusion
The treatment approach depends on the underlying cause, severity of symptoms, and the amount of fluid accumulated. Options include:
- Observation: Small, asymptomatic effusions may only require regular monitoring.
- Medications:
- Anti-Inflammatory Drugs: To reduce inflammation (e.g., NSAIDs, corticosteroids)
- Antibiotics or Antifungals: If an infection is identified
- Pericardiocentesis: A procedure to drain excess fluid using a needle, guided by imaging techniques
- Surgical Intervention:
- Pericardial Window: Creating an opening in the pericardium to allow continuous drainage
- Pericardiectomy: Removal of part or all of the pericardium, typically in recurrent cases
Timely diagnosis and proper medical intervention are essential for treating pericardial effusion which is a serious medical condition. The optimal treatment comes from a trusted heart hospital in Delhi. The cardiac specialty division at Primus Super Specialty Hospital in Delhi has the latest medical equipment and specialized cardiac specialists. Patients who display signs of heart fluid effusion and their family members should immediately seek medical consultation from an experienced cardiologist in Delhi for comprehensive care.